Treatment
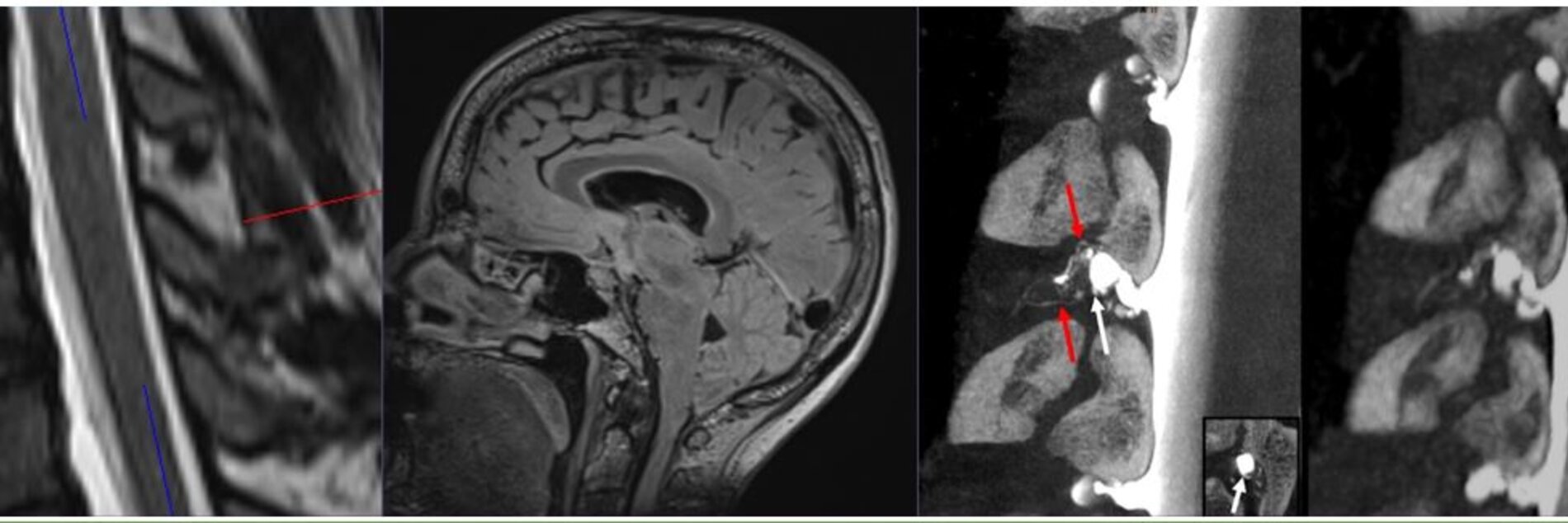
Spontaneous Intracranial Hypotension (SIH)Regardless of the therapy chosen, we recommend conducting clinical and imaging monitoring.
Non-targeted Epidural Blood Patch (EBP) - Department of Neuroradiology:
In this method, a person's own blood is introduced into the lower spinal canal outside the meninges (Dura). This is referred to as epidural.
Non-targeted means that there is no attempt to directly target the actual leak, which is usually located elsewhere. Instead, by introducing a large volume of blood, the dural sac is constricted, which can already significantly alleviate the symptoms.
An EBP is the first, and fasted approach to treat SIH. It can facilitate the natural healing process. Nevertherless, data showes persistent leaks in >70% of the cases (Piechowiak et al.)
In our center, this method is performed under fluoroscopy with subsequent bed rest.
Targeted Patch (Blood/Fibrin) - Department of Neuroradiology:
Once the leak has been localized, a targeted patch with the goal of sealing the leak can be attempted. In our center, this method is primarily used in the treatment of sacral leaks, and CSF-venous fistulas.
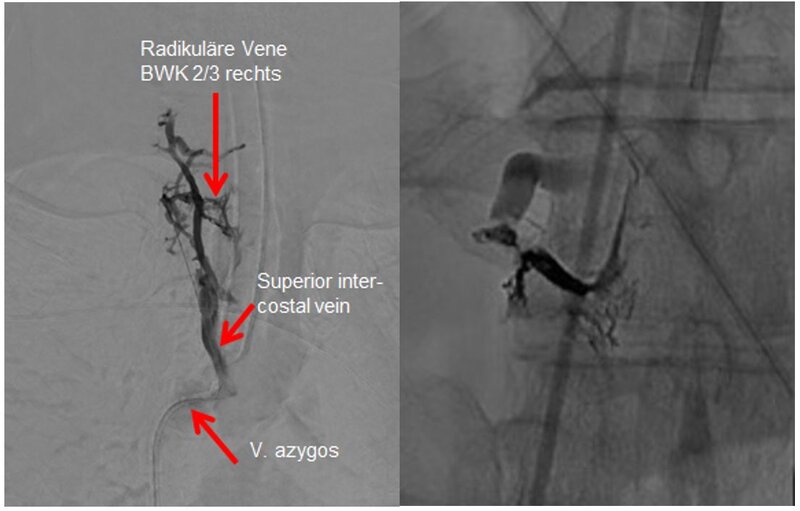
Embolization - Department of Neuroradiology:
Cerebrospinal venous fistulas (Type III) can be closed using interventional embolization in catheter technique. In this procedure, a catheter is inserted into a large vein in the groin, the fistula is located, and then sealed with a special adhesive. This procedure can be performed under general anesthesia or, in some cases, under local anesthesia.
Patients may be discharged as early as the following day, or the day after.
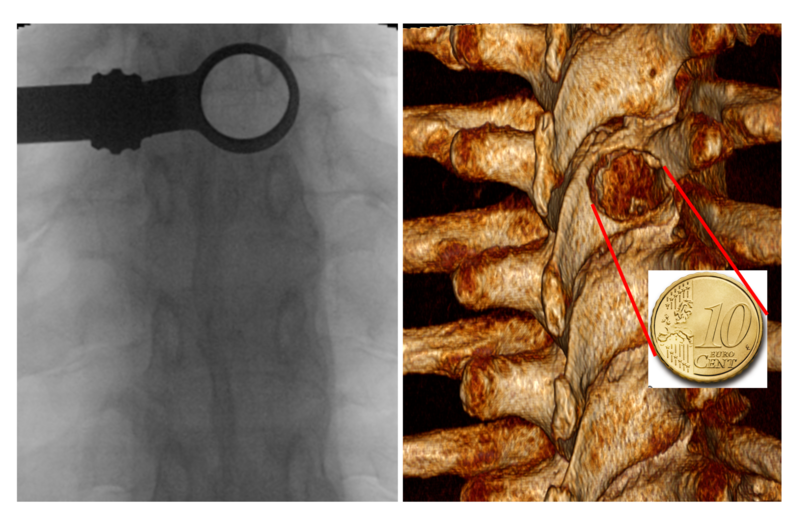
Work Tube (X-ray image on the left) with a diameter of 20mm. The size of the bone defect is approximately comparable to a 10-cent coin.
Surgery - Department of Neurosurgery:
Surgical closure of a spinal CSF leak can be performed in ventral and lateral CSF leaks, also in CSF-venous fistulas. It ist teh most definite way to seal a leak.
Using state-of-the-art minimally invasive neurosurgical techniques, a pre-located CSF leak can be identified and sealed. The access point or incision is always made on the back side at the level of the leak, regardless of the leak's location within the circumference of the dura and the type of leak. This approach allows us to minimize the invasiveness of the surgical procedure and, consequently, the rate of complications. The actual closure of the leak is tailored to the specific type of leak.
As of August 2023, with over 300 procedures performed at the University Medical Center Freiburg, there have been no new severe neurological deficits. The revision rate (the need for a repeat procedure) is currently approximately 4%.
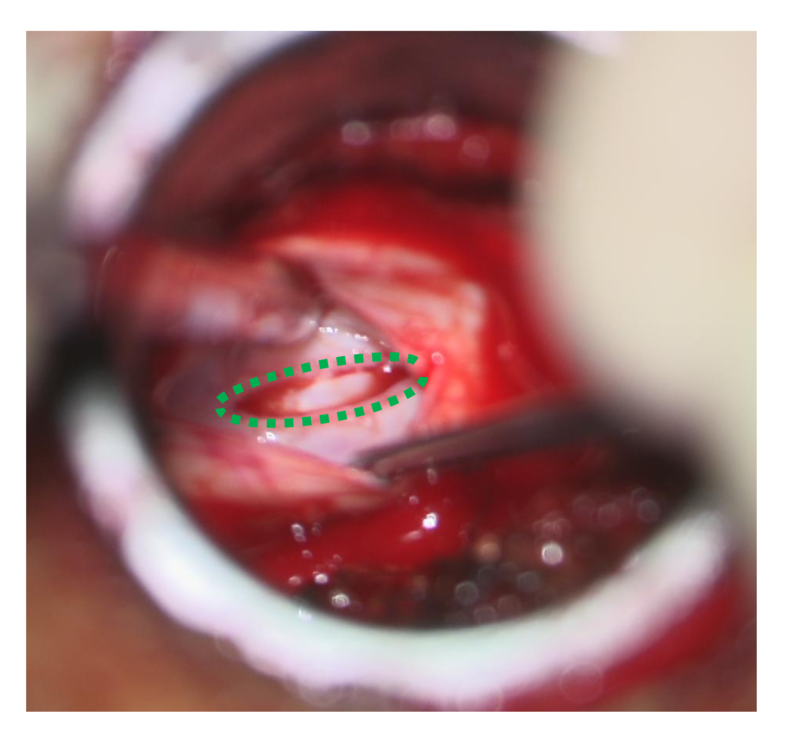
View through the surgical microscope: The defect in the dura is approximately 4mm (green, Type 1 ventral leak).
What should be considered after surgery?
As a general rule, mobilization can usually begin on the first day after surgery. Rotations of the back, especially when carrying heavy objects, should be avoided for several weeks. In most cases, all other movements, including moderate physical activities, can be resumed promptly. Patients will receive more detailed instructions following the procedure.
Am I fully recovered after the procedure?
After an embolization or surgery, healing is not immediate. The entire recovery process typically takes several weeks to months.
It's important to note that circulations need time to readjust, both in terms of cerebrospinal fluid and cardiovascular regulation, especially after an extended period of lying down.
Some patients may develop rebound hypertension after treatment. This can be temporarily treated with medication, such as acetazolamide. In most cases, low dosages and a limited time of treatment are sufficient to control the symptoms. In rare cases, permanent treatment may be necessary. In such cases, other causes of intracranial hypertension should be considered.
The psychosocial burden that occurs during and after the illness should not be underestimated.
The often lengthy duration of the illness, frustrating doctor visits, misdiagnoses, and inadequate treatments also represent a psychological burden. The working environment and social life are affected. Patients also need time to recover from these challenges.
Here, you can find guidelines for the treatment of SIH.
You can read more information about our interdisciplinary CSF team, our diagnostic capabilities, and treatment options on these pages.
You can find contact information here.
Additional informational materials and useful links can be found here.
Klinik für Neurochirurgie
im Neurozentrum
Breisacher Straße 64
D-79106 Freiburg
Telefon: 0761 270-50010 /-50020
Telefax: 0761 270-50240
neurochirurgie@uniklinik-freiburg.de
Prof. Dr. Jürgen Beck
Ärztlicher Direktor
Telefon: 0761 270-50060
International call: +49-761-270-50060
j.beck@uniklinik-freiburg.de

André Doherr
Pflegedienstleiter
Telefon 0761 270-52260
Telefax 0761 270-54200
andre.doherr@uniklinik-freiburg.de
Moritz Wenk
Verwaltungsreferent
Augen- / HNO- Klinik / Neurozentrum
Telefon 0761 270-40650
moritz.wenk@uniklinik-freiburg.de