Postdural puncture Headache (PDPH)
What does PDPH mean?
Postdural puncture headache (PDPH) is a secondary headache, thus, a headache caused by a specific reason.
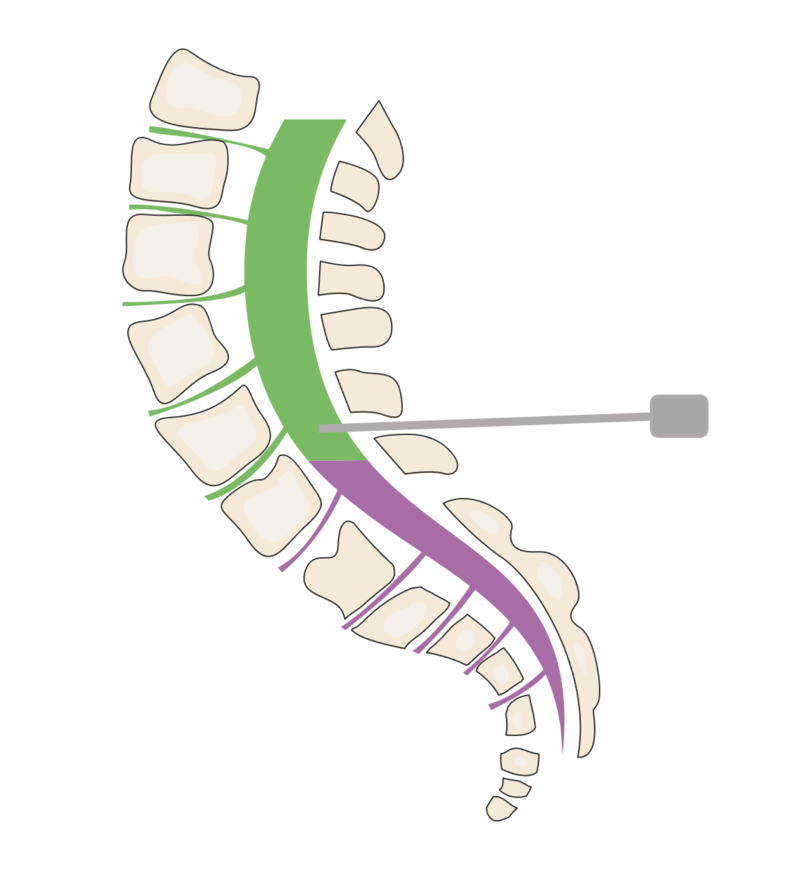
PDPH can occur when the tough outer membrane of the layer surrounding spinal cord, nerves, and CSF space (Dura) is punctured in the area of the lower back.

How is PDPH diagnosed?
Typically, this headache occurs within 5 days after intentional or unintentional puncture. However, later onset, chronic courses, and atypical clinical presentations have also been described and are often underestimated.
Most patients complain of a new headache, often located more in the back of the head and neck. These symptoms occur or worsen when standing up. When lying down, the discomfort significantly improves or even disappears completely.
In addition, there are many other various symptoms such as nausea, vomiting, dizziness, auditory and visual disturbances, sensory disturbances, sensitivity to noise and light, concentration difficulties, and many more.
Imaging is normal - does it mean I am imagining?
The diagnosis is established by the correlation between the onset of headaches with typical features and the puncture.
In some cases, changes in routine MRI can be observed (similar to SIH). A normal MRI does not rule out PDPH.
We recommend the following MRI examination in patients with refractory symtpoms:
Head MRI: 1mm MPrage post-contrast, axial 1mm CISS, or 2mm T2 fs over the orbits.
Spine MRI: At least 1mm 3D T2 SPACE fs over the lumbar spine.
How are the risks to develop PDPH?
The incidence of PDPH varies widely, depending on patient (e.g., age, sex, pregnancy, body mass index [BMI]) and procedural risk factors (e.g., needle size and type, bevel orientation for cutting needles - largely reduced risk by using pin-point non-cutting needles as compared to cutting needles) . The estimated incidence of PDPH of diagnostic lumbar punctures lies at 3-11 percent of cases, depending on the type and size of needle used.
PDPH is the most common complications of a lumbar puncture performed for diagnostic purposes. It also occurs after accidental dural puncture during routinely performed medical procedures like epidural pain relief for parturients, spinal regional anesthesia.
Predominantly, PDPH is seen by unintentional dura puncture in providing obstetric anesthesia and analgesia in parturients.
Can PDPH be treated?
Yes, PDPH can be treated, and it should be treated.
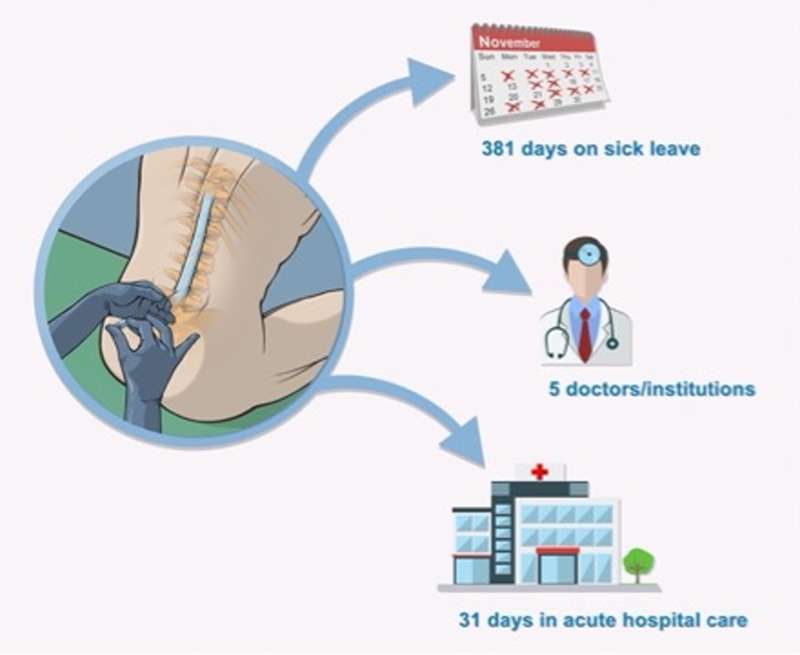
A common problem is that PDPH is not treated early enough, nor adequately.
The frequency of chronic courses is underestimated.
Especially after epidural anesthesia (PDA) and childbirth, two patients suffer simultaneously: the mother and the child.
Rest, drink, wait?
If the symptoms do not improve promptly and significantly with the necessary immediate measures (pain therapy, fluids, lying down, caffeine), a sufficiently large-volume bloodpatch should be administered (see consensus guidelines below).
A blood patch can also be repeated if its effect is not sufficient, or not lasting.
There are various other pain management methods, the evidence for which is not yet fully established, and they may be performed in addition based on the center's experience (analgesia of N. occipitalis, sphenopalatine block).
In rare cases where the basic treatment is ineffective, the remaining open leak might be closed through surgery.
Am I fully recovered after the procedure?
After an epidural bloodpatch, and even after successful surgery, complete healing is not immediate. The entire recovery process typically can take up to several months, in rare cases even years.
It's important to note that circulations need time to readjust, both in terms of cerebrospinal fluid and cardiovascular regulation, especially after an extended period of lying down.
Some patients may develop rebound hypertension after treatment. This can be temporarily treated with medication, such as acetazolamide. In most cases, low dosages and a limited time of treatment are sufficient to control the symptoms. In rare cases, permanent treatment may be necessary. In such cases, other causes of intracranial hypertension should be considered.
Additionally, all typical methods of symptomatic treatment need considering that need to be tailored to the symptomes being percieved as the most severe.
The psychosocial burden that occurs during and after the illness should not be underestimated.
The often lengthy duration of the illness, frustrating doctor visits, misdiagnoses, and inadequate treatments also represent a psychological burden. The working environment and social life are affected. Patients also need time to recover from these challenges.
Here, you can find guidelines for the treatment of PDPH.
You can read more information about our interdisciplinary CSF team, and find contact information here.
Additional informational materials and useful links can be found here.
Here you can find general informations and instructions regarding
Klinik für Neurochirurgie
im Neurozentrum
Breisacher Straße 64
D-79106 Freiburg
Telefon: 0761 270-50010 /-50020
Telefax: 0761 270-50240
neurochirurgie@uniklinik-freiburg.de
Prof. Dr. Jürgen Beck
Ärztlicher Direktor
Telefon: 0761 270-50060
International call: +49-761-270-50060
j.beck@uniklinik-freiburg.de

André Doherr
Pflegedienstleiter
Telefon 0761 270-52260
Telefax 0761 270-54200
andre.doherr@uniklinik-freiburg.de
Moritz Wenk
Verwaltungsreferent
Augen- / HNO- Klinik / Neurozentrum
Telefon 0761 270-40650
moritz.wenk@uniklinik-freiburg.de