Hemangioblastomas and von Hippel-Lindau (VHL) disease
Hemangioblastomas
What is a hemangioblastoma?
Hemangioblastomas of the central nervous system are benign tumors. They mostly occur in the posterior fossa or spinal cord. These tumors can develop sporadically or hereditarily as a manifestation of von Hippel-Lindau disease. Typically, the tumors develop an adjacent tumor-associated cyst as a small, solid formation along the wall of a large cyst. These cysts contain an amber-colored liquid and in some cases form a so-called syrinx in the spinal cord.
What are the symptoms of these benign tumors?
Symptoms of hemangioblastomas in the cerebellum mainly include headaches, nausea, incoordination, unsteady gait and dizziness. In progressive tumors it can also lead to disorders of consciousness. Patients affected by tumors of the spinal cord may develop numbness or paralysis. In addition, an unsteady gait may occur. Difficulties with defecation and urination are some of the other possible symptoms. The tumors rarely cause pain.
Nationwide Center for hemangioblastoma surgery
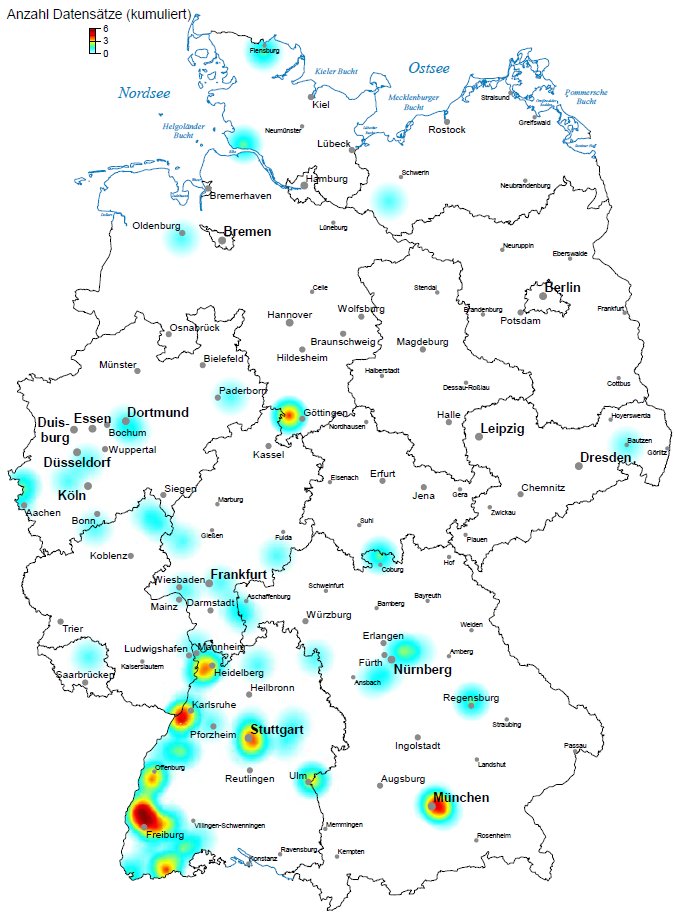
Survey period of the illustration: 04/2016 - 03/2017
Download this map in large format as PDF (450 KB)
Every year we are in charge for more than 100 patients with the rare von Hippel-Lindau (VHL) disease and hemangioblastomas from all over Germany.
What is the medical treatment?
In general, the tumors grow slowly so that an annual check-up is sufficient. For the primary diagnosis and follow-up examination, an MRI with contrast is the method of choice. If treatment is necessary, the tumor is removed microsurgically. Since hemangioblastomas are benign tumors, the tumors can usually be completely removed and generally do not recur. Radiation therapy has so far provided no convincing evidence of success. Drug therapy methods are currently the subject of scientific investigation. There is currently no drug that has been shown to be effective against hemangioblastomas.
von Hippel-Lindau (VHL) disease
What is von Hippel-Lindau disease?
VHL is a hereditary tumor syndrome named after doctors Eugen von Hippel and Arvid Lindau who discovered the disease in the early 20th century. Besides hemangioblastomas, the VHL disease can cause tumors of the retina (retinal angiomas), renal tumors and tumors of the adrenal gland (pheochromocytoma). In addition, tumors in the inner ear, the epididymis and the pancreas can occur.
What is the treatment for von Hippel-Lindau disease?
Patients affected by VHL disease usually develop multiple hemangioblastomas. This circumstance must be taken into consideration in the surgical treatment. Because the appearance of new tumors has always to be expected, a definitive cure is not possible surgically. Although the removal of hemangioblastomas of the CNS is usually carried out without long-term damage, the removal of all tumors in patients with VHL disease is not considered the most reasonable option. For these reasons, the following procedure is considered most reasonable: patients with VHL disease are monitored by annual MRI of the brain and spinal cord. It is then discussed individually which tumors should be removed. Generally, it is advisable to remove those hemangioblastomas which cause discomfort. In asymptomatic tumors that grow in size and develop a tumor-associated cyst over the course, we mostly recommend removal. This is based on comparisons we made in the state of a large number of patients before and after surgery. This comparison demonstrated that there is generally no change in complaints of functionality. Although this means that no permanent damage is normally caused by an operation, it was found that any issues that did occur before surgery could no longer be corrected by surgery. We therefore consider it most ideal to remove the tumors at a time when they cause no discomfort. Therefore, we do still operate on tumors that are (still) asymptotic but show growth.
How do I know that I have a hemangioblastoma?
Hemangioblastomas in the cerebellum are often symptomatic with headaches. Everyone has occasional headaches, but if the pain changes in nature or intensity and steadily increases, this can be indicative for tumor growth. Later, nausea and vomiting occur. Furthermore, incoordination occurs in tumors of the cerebellum. Spinal cord tumors may cause disturbance in gait, numbness, paralysis or pain.
Which tumors need surgery? Is it possible to wait?
The decision for surgery is always made on an individual basis. There are two typical situations in which we recommend an operation: if a tumor causes complaints or if an asymptomatic tumor increases in size and consumes space.
How do I prepare?
Please, bring the following with you: your personal items, a briefing of your family doctor and a list of your medications. If you are in treatment for other diseases, please bring any findings. Particular findings on cardiovascular and respiratory conditions are important to the anesthesiologist. You should also bring any X-ray, CT and MRI images available to you. This is important for the operation.
How long will I be in hospital?
About a week. On the first day you will be examined and prepared for the operation. The operation generally takes place on the second day. Our patients are discharged usually on the 5th day after surgery. Please arrange in advance any necessary help from relatives or friends for the first few days when you get home.
Is the operation dangerous?
Hemangioblastomas are different from other tumors because they are very well supplied with blood. This makes them a little more difficult to operate than other tumors. If the surgeon is set to, the operation is generally not dangerous, and is a routine procedure. However, it is recommended that the operation be carried out in a larger center with extensive experience in dealing with hemangioblastomas.
Will I need rehabilitation after the operation?
No, not generally. Rehabilitation is generally not required after the surgery of tumors in the cerebellum. In about 20% of cases, patients undergoing surgery on a tumor in the spinal cord or brain stem temporarily experience slight difficulty walking. In this situation, it is advisable that we organize rehabilitation for you.
When can I fly for holidays after the surgery?
After surgery for brain tumors, you should wait about 4 weeks before flying. This is due to the fact that air can accumulate in the head, which can expand when under negative pressure, and also due to the increased risk of thrombosis.
What may I do after surgery?
After brain surgery, you may not drive a car for 3 months because seizures can occur in rare cases. Otherwise, there are no formal prohibitions. Start slowly and gradually after surgery in pursuing your daily activities. You will see for yourself what works for you and what does not.
How long does it take until the wound has healed?
After 10 days, the staples or sutures can be removed. Two days later, your hair can be washed. Wound healing continues for several weeks. Direct sunlight on the wound should be avoided. It takes several months for the bone flap to fuse with the skull. Contact sports should be avoided for 3 months.
Where can I get more information?
You get more information from the head of the von Hippel-Lindau disease specialists during weekdays by phone (+49 761 270-50010). Please also see the printable flyer below on this page. Further, conversation with other patients can be helpful. For this reason, a support group is available, the "Verein VHL (von Hippel-Lindau) betroffener Familien e.V." www.hippel-lindau.de
Consultation information:
Special consultation for von Hippel-Lindau disease
Donwloads
Flyer "Specialities VHL / hemangioblastomas" (PDF file, 1.5 MB, in German)
Links related to the von Hippel-Lindau disease
Central Coordinator of the VHL disease:
PD Dr. Stefan Zschiedrich, Internal Medicine IV
Self-help groups:
www.hippel-lindau.de
www.vhl.org

Prof. Dr. J.-H. Klingler, MD
Senior neurosurgeon

Dr. Christine Gizaw, MD
Attending neurosurgeon


