Research
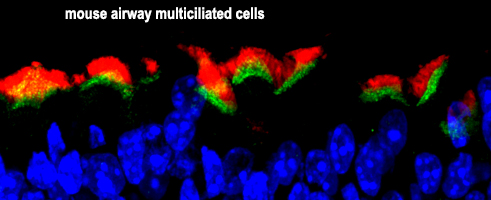
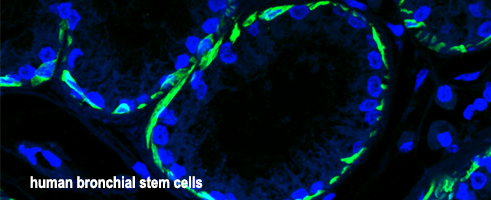
Our research aims to understand mucociliary epithelial development, homeostasis, disease and regeneration
We use cell, developmental and molecular biology approaches to understand how mucociliary epithelia are formed in development, how they are maintained in a healthy state during homeostasis or which changes lead to disease, and which mechanisms are employed during mucociliary regeneration. By analyzing different layers of molecular regulation at the single cell as well as at the tissue-wide level, we integrate various types of data to gain a more holistic understanding of mucociliary epithelial self-organization mechanisms. This knowledge is then used for airway disease modeling in model organisms and tissue culture, to generate organoid models for diagnosis and drug development, and to manipulate cells to create designed epithelia with novel biological propoerties.
Through that, we learn about the principle mechanisms of tissue formation and generate data with translational value for ciliopathy and chronic airway disease patients.
Ciliopathies are diseases in which cilia are either not correctly formed or in which cilia function is impaired. Many different types of ciliopathies are known, they can affect every organ (e.g. brain, kidney, lungs, reproductive organs, eyes, etc.), and are mostly affecting multiple organ systems simultaneously. Ciliopathy patients frequently suffer from airway infections, impaired smell, taste and vision, cognitive disabilities, kidney failure, obesity and infertility. By investigating how different genes regulate the specification of ciliated cells and how gene products contribute to normal cilia formation/function in cells, we provide a better knowledge base for clinicians, that helps them to diagnose and treat the disease.
If you want to find out more about ciliopathies, https://www.ciliopathyalliance.org provides a nice overview and additional resources for patients and familiy members. If you are a researcher and want to take a look at the growing ciliopathy literature, please follow this link to pubmed: "ciliopathy" at pubmed.
Chronic airway diseases and lung cancers are among the most common causes of death worldwide (WHO report), and the number of cases are increasing. Chronic obstructive pulmonary disease (COPD), asthma, idiopathic pulmonary fibrosis and various lung cancers cause changes in the composition and function of airway mucociliary epithelia. These changes alter cell type composition, motile cilia function, ion balance and mucus secretion in the respiratory tract. Mucociliary clearance, a mechanism that removes inhaled particles and pathogens from the lung, relies on correct cell type composition, cilia function, ion balance and an appropriate mucus secretion. If defects in any of these functions arise, mucociliary clearance fails, which leads to airway obstruction, problems breathing and in gas exchange, and increases the risk for lower respiratory infections (e.g. pneumonia). We study the mechanisms that regulate cell type composition and cilia function, how cell cell communication is employed in development and how it is altered in disease, and how transcription factors, post-transcriptional regulation, and epigenetics regulate genes involved in tissue formation, cilia motility, ion homeostasis and mucus secretion.
If you want to learn more about chronic airway diseases, the WHO provides a nice entry point: chronic airway disease at WHO. If you are interested in the growing literature on chronic airway diseases, please follow the pubmed link: "chronic airway disease" at pubmed.

In our research, we use a wide range of in vivo and in vitro models.
- Planaria: These are flatworms with a remarkable ability to regenerate. Planarians use a mucociliary epidermis on the ventral surface to move. Thus, planaria "surf" on a secreted mucus layer using the motile cilia of multiciliated cells.
- Basal fish (e.g. sturgeon): In contrast to modern fish, which have lost their mucociliary epidermis, basal fish have an embryonic mucociliary epidermis similar to Xenopus.
- Xenopus frogs: Frog embryos are our main model organism. They develop fast, establish a mucociliary epidermis very early during development (the first functional organ!), and because they have an airway-like mucociliary epithelium on their skin, cells are easy to manipulate and to image. In addition to the epidermis, we are also analyzing cilia in the left-right organizer, the developing central nervous system and in the foregut.
Read more about the power of Xenopus for cilia and mucociliary research here: review article 1, review article 2.
Xenopus resources: Xenbase - model organism database, NXR - national Xenopus resource (USA), EXRC - European Xenopus resource center (UK), CRB - Centre de Ressources Biologiques Xénopes (F), NBRP - Japanese Xenopus tropicalis rescource.
- Mice: Mice are commonly used to study mammalian airway epithelia in vivo. We also take advantage of the powerful genetic tools available in mice, but we are focusing our mouse research to the confirmation of mechanisms that we have first elucidated in Xenopus and other organisms. Thereby, we are minimizing the number of animals used in research and promoting the 3R-principles in animal research.
3R-principles: If you want to know more about Replacement, Reduction and Refinement for the ethical use of research animals, please visit the website of the European Union for description and how it is implemented in biomedical research in the EU.
- Human: We learn a lot for our projects from the findings clinicians make when they diagnose and treat human patients. Furthermore, we employ in vitro cultures using primary airway cells or immortalized human airway stem cells as starting point. These cells can be either cultured using air-liquid-interface (ALI) planar cultures or as 3D-organoids when these cells are grown in an artificial extracellular matrix.



